Marcus Fatunmole (Abuja)
It was altogether a good and bad year for Nigeria’s health sector in 2018. Three years into the administration of President Muhammadu Buhari, the much expected ‘change’ has arguably not berthed on the sector.
Crisis at the National Health Insurance Scheme (NHIS) was one of the unpleasant incidents that characterized the nation’s health system in 2018. The crisis, which began in 2017, reached a crescendo when the governing board of the scheme through its chairman, Dr Enyatu Ifenne, suspended the Executive Secretary of the scheme, Prof. Usman Yusuf, on October 18, over alleged corrupt practices.
Yusuf, who had in 2017 been suspended by the Minister of Health over similar allegations and was subsequently reinstated by president Buhari, refused to heed the council’s directive.
The crisis polarized employees of the organization. While some stood with the council, others backed the adamant ES who continued in office with the help of gun-wielding policemen and operatives of the Directorate of State Services.
President Muhammadu Buhari eventually waded in two weeks later, directing the ES to proceed on administrative leave, while the panel he set up probes him. The panel submitted its findings on Monday December 24, while the nation awaits the President to implement the report, as promised by Secretary to the Government of the Federation, Boss Musptapha, who received the report on behalf of the president.
One of the good moments in Nigeria’s health sector was the launch of Community Health Influencers, Promoters and Services (CHIPS) in Lafia, Nasarawa state by President Muhammadu Buhari on Tuesday February 6, 2018.
CHIPS, according to Executive-Director, National Primary Health Care Development Agency (NPHCDA) Dr Faisal Shuaib “aims at improving access and equitable coverage to essential health services, with focus on maternal, new born and child survival.”
Despite its launch by the president, it has not been adopted by most states in the country as planned. Though CHIPS was federal government’s initiative, it was expected to be driven by the states which will determine the allowances to be paid the employees.
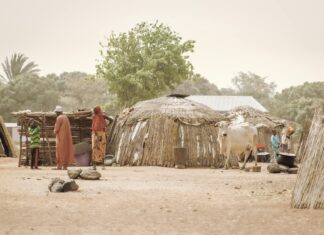
The launch of CHIPS became necessary following increasing loss of confidence in the nation’s primary health centres (PHCs); lack of access to the facilities and shortage of manpower.
The Federal Government also pledged to launch a free health care for mothers and children in the country. It was expected to be launched before the end of the year, but it wasn’t.
No doubt, Nigeria’s health sector is driven by donor funds, as grants for HIV/AIDS alone by the World Bank, Global Fund, and UNIAIDS near Federal Government’s annual budget for the sector.
In Nigeria, health is on the Concurrent List of the constitution, which implies that both Federal and State governments are responsible for provision of health care, and could develop policies independently for the health of the people.
The Federal Government owns and manages 20 Federal Teaching Hospitals, 22 Federal Medical Centres and 13 Specialist Hospitals. Hundreds of secondary health facilities are owned and managed by states, while thousands of primary health facilities jointly managed by states and local governments spread across the nation’s 36 states.
It is generally assumed that most states, except Lagos, Bauchi, Kaduna and few others, perform below expectation in health care services in the country. The states and local governments are responsible for the running of primary health care services while the Federal Government provides needed coordination, support and guidance.
But, the state of many of the PHCs is so terrible that they are occupied by goats, dogs and other domestic pets. This arises from years of neglect, much reliance on tertiary health facilities and extremely poor funding by successive governments.
In 2018, the Federal Government budgeted N8.6trillion for its fiscal year, out of which it devoted N340.456 billion to the Federal Ministry of Health.
The recurrent budget of the ministry jumped by six percent from 2017’s N253.8bn to N269.3bn in 2018, while capital budget rose from N55.6 billion in 2017 to N71 in 2018.
N55 billion was also approved by the executive, in compliance with the National Health Act which stipulates that one percent Consolidated Revenue of the federation be allocated to the health sector. The Act was signed into law in December 2014 by former President Goodluck Jonathan, and that portion of the law was never implemented since then.
However, details of health budget releases to health agencies by the government are not available to this newspaper at the time of filing this copy, but government style of lumping statutory transfers together often makes it difficult for the public to quickly dissect how much is being released to specific agencies. Marginal increase in health budget could only correspondingly boost a sector that has been riddled with challenges for decades.
Statistically, as at the end of 2018, Nigeria trails behind most nations of the world in health. According to 2015 Joint Monitoring Programme (JMP) of World Health Organization and UNICEF, of estimated 180 million Nigerian population, 46 million practice open defecation, while 130 million use an unimproved sanitation facility, with more than half living in rural areas.
45,000 children under five die annually in Nigeria from diseases caused by poor access to water, sanitation and hygiene (UN-GLAAS, 2014)
Nigeria retains its position as the world’s leader in malaria burden, contributing about a quarter of global burden of the disease, and about the same measure in Africa.
It also retains its place as second most leading nation in HIV/AIDS epidemic, globally, trailing South Africa. Meanwhile, the number of persons living with the disease, who have been place on antiretroviral drugs, increased by about 200,000 within the year.
Since health is wealth, Nigeria’s population currently projected by the National Population Commission at 198 million is being described as a disaster in waiting. Experts, including Chairman, Association for the Advancement of Family Planning, Dr Ejike Oji, said at the just concluded 5th National Family Planning Conference that the nation’s population might attract more harm than good. The experts based their arguments on the fact that rather than achieve demographic dividends through adequate planning for its population, Nigeria faces unemployment, crimes, unplanned births among others that would readily harm its future.
It is estimated that 58,000 women die annually in the country from birth-related complications, 1/22 women in the country, according to Mamaye, a health non-governmental organization, risks dying from maternal cause; while 27 new-born die every hour, according to the organization. There are persistent cases of girl-child mutilation, child marriages resulting in diseases such as fistula among others.
In accessing heath care, most Nigerians pay out-of-pocket. The National Health Insurance Scheme covers only about six percent of the nation’s population. Over 60 percent of services are rendered by private facilities, and majority of citizens who live on less than two dollars a day could not afford the bills.
Good news: one unique feature of Nigeria health system in 2018 was relative peace among the workforce. Unlike the past where strikes were alternated among the unions in the sector in bids to show might and power, leadership of the Nigeria Medical Association (NMA) has repeatedly made it clear to all that only a lasting peace would be tolerable in the sector.
One of major breakthroughs in the nation’s health system was the successful separation of Siamese twins by the University of Abuja Teaching Hospital, Gwagwalada, Abuja within the year.
The nation consolidated its effort to prevent disease outbreaks and confront them where they do occur by having a law establishing its National Centre for Disease Control (NCDC) signed into law by President Muhammadu Buhari.
Whereas the hype that characterized activities of National Agency for Food and Drug Administration and Control, NAFDAC, in past years reduced within the year, the agency continued in its efforts to safeguard the lives of people of the nation by confiscating illicit, counterfeit, and contraband foods and drugs.
The Director-General of the agency, Prof. Mojisola Adeyeye, however dropped a bombshell when she led Senate Committee on Health on tour round facilities of the agency in Lagos in November 2018.
She said: “80 per cent of our equipment is no longer working and that is a major challenge to deliver on our mandate. The last time, the World Health Organisation visited our laboratory in Yaba, they scored us zero.”
As at the end of 2018, the National Institute of Pharmaceutical Research and Development (NIPRD) was yet to get desired attention from government. NIPRID and National Institute for Medical Research (NIMR) are supposed to lead Nigeria into medical breakthrough (both traditional and orthodox)
The world expect the nation to do more and improve its health as the journey into 2019 begins.