By Martins Idakwo
On the 29th of Aprill 2020, the death of Former Civilian Governor of Borno State, Muhammad Goni, was announced after falling ill. Umar Goni had announced it on behalf of the family.
‘’Our dad was sick around 9-10pm, we rushed him to the hospital and to my surprise we couldn’t find a single doctor”. He stated.
He added that ‘’None of the consultants were around to attend to him, once they tell them a patient is around, they run, thinking he’s a Covid-19 patient. We couldn’t get a bed, we couldn’t get even first aid.’’ He continued. He was tossed from one hospital to another until he eventually died.
Mr. Goni was elected governor of Borno State in 1979. He governed the state until 1983 when he lost his second term bid.
Considered by many as one of the best governors of the state, Mr. Goni continued to enjoy the respect and admiration of the people for his past glory.
He contested for the governorship of Borno State in 2011 under the Peoples Democratic Party (PDP) and lost the keenly contested election to former governor Kashim Shettima, now a senator. This is the sad and pathetic tale that came out from Borno State.
Yes, he was a former governor of the state and this still happened to him.
Under the Nigerian law, a doctor has a duty to save the life of a patient whose refusal of medical treatment will inevitably lead to death, not to talk of the one seeking medical attention, but Goni was left to die.
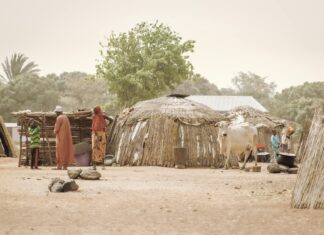
There’s no doubt that the Nigerian healthcare has suffered several down-falls. Despite Nigerian’s strategic position in Africa, the country is greatly underserved in the healthcare sphere. Health facilities (health centers, personnel, and medical equipment) are inadequate in the country, especially in rural areas.
While various reforms have been put forward by the Nigerian government to address the wide ranging issues in the health care system, they are yet to be implemented at the state and local government levels.
Perhaps, the biggest danger faced at the moment is panic. To control diseases such as COVID-19, it is critical that human behavior is controlled in a way that inhibits the spread of the disease. The challenge with panic is that people change their behavior erratically.
They might even behave in a way that leads to the disease spreading, or poses a different risk entirely to them and their communities.
Misinformation can lead to panic. In fact, it does more than create panic. It can lead to wrong actions. We have already seen people come down with chloroquine toxicity in this pandemic when they heard the drug might be effective.
Misinformation can also lead to complacency. There are people who believe that Covid-19 can’t come to them, and do nothing to prevent it.
Before COVID-19 became part of the equation, 35% of the health facilities in Adamawa, Borno and Yobe states were damaged by the conflict, according to the World Health Organization (WHO). As a result of the lack of access to healthcare, people die of preventable and treatable diseases like malaria, measles and cholera.
The potential effect of the coronavirus, which has overwhelmed some of the best healthcare systems in the world, worries many health specialists. But healthcare workers in the northeast of Nigeria face an additional threat – being attacked.
In the midst of the coronavirus pandemic, medical emergencies unrelated to COVID-19 still occur. Hassan, who works at two hospitals in the FCT, is among a number of doctors who worry that people experiencing warning signs of life-threatening conditions are delaying seeking emergency help, out of fear of going to coronavirus-strained emergency rooms.
An average of 20,000 Nigerians travel to India each year for medical assistance due to the absence of a solid healthcare system at home.
“Nigeria is responsible for a high amount under-five child deaths.” UNICEF said, in a recent repot that “preventable or treatable infectious diseases such as malaria, pneumonia, diarrhea, measles and HIV/AIDS account for more than 70% of the estimated one million under-five deaths in Nigeria.”
Another report by the WHO says that nearly 10% of newborn deaths in the world, last year, occurred in Nigeria. Furthermore, five countries accounted for half of all newborn deaths, with Nigeria third on the list. These are India (24%), Pakistan (10%), Nigeria (9%), the Democratic Republic of the Congo (4%) and Ethiopia (3%). Most newborn deaths occurred in two regions: Southern Asia (39%) and sub-Saharan Africa (38%).
Total number of Covid-19 cases in Borno stands at 250, recovered cases is 141, while deaths is at 25.
In conclusion, policy makers and political actors need to devise healthcare reforms to address the lack of social and financial protection for the poor and vulnerable populations. Part of this reform is the expansion of the NHIS.
States should be mandated to provide health insurance coverage to all residents. Making health insurance optional for states over the years has affected the ability of the NHIS to increase the level of coverage for the people.
The availability and the affordability of healthcare challenge most countries. The global shortages and unequal distribution of qualified health personnel are a major constraint in providing universal access to healthcare.
Wide-spread reforms of health systems are continuously changing the employment environment for healthcare workers.
Just like Mr. Muhammad Goni, nobody should die from ordinarily curable or even life-threatening disease. If Goni could be left to die carelessly regardless of his status and caliber in the society, then what is the hope of the common man?